FREMONT, Calif., Aug. 31, 2016 /PRNewswire/ — Asterias Biotherapeutics, Inc. (NYSE MKT: AST), a biotechnology company focused on the emerging field of regenerative medicine, today announced that its Data Monitoring Committee (DMC) has reviewed the safety data from the initial cohort of three patients dosed with 2 million cells, and a subsequent five patients in the second cohort dosed with 10 million cells, and has cleared the company to now begin dosing a third cohort of 5-8 complete cervical injury patients (AIS-A patients) with the highest dose of 20 million cells. Concurrently, the study is also proceeding with enrolling the first cohort of 5-8 sensory incomplete cervical spinal cord injury patients (AIS-B patients), each of whom will be administered 10 million cells.
The SCiStar study is an ongoing Phase 1/2a clinical trial funded in part by a $14.3 million grant from the California Institute for Regenerative Medicine (CIRM) and is designed to evaluate the safety and efficacy of escalating doses of AST-OPC1 in newly injured patients with sensory and motor complete cervical spinal cord injury (SCI), as well as newly injured patients with sensory incomplete SCI. These patients are commonly referred to as AIS-A and AIS-B patients, respectively. The results of the ongoing trial continue to support a positive safety profile for AST-OPC1. There have been no serious or unexpected adverse events related to AST-OPC1, the administration procedure or the accompanying short course of low-dose immunosuppression in any of the patients treated with AST-OPC1, including five patients in an earlier Phase 1 trial with neurologically complete thoracic SCI.
“The positive safety data in the previous phase 1 study and in the ongoing phase 1/2a study gives us the confidence to now proceed to administration of 20 million cells, which based on our significant pre-clinical research is likely well within the dosing range where we would expect to see clinically meaningful improvement in these patients,” said Dr. Edward Wirth, Chief Medical Officer of Asterias Biotherapeutics.
The data set evaluating the efficacy results six months after implantation of 10 million AST-OPC1 cells in complete cervical spinal cord injury patients will be available in January 2017 and will focus on improvement in physical functioning of the upper extremities (fingers, hands and arms) of each treated patient utilizing scoring on the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI scale). The published literature and opinion leaders in the spinal cord injury field indicate that a two motor level improvement in functioning utilizing this validated scale is clinically meaningful for these patients and should be the key measure in the evaluation of new therapies.
“According to the published scientific literature as well as key opinion leaders that we speak to, a two motor level improvement in physical functioning on the ISNCSCI scale can translate into a significant improvement in quality of life, reduced need for daily care and increased ability to live independently for patients with cervical spinal cord injuries. We look forward to announcing the six month follow up data from this 10 million cell cohort in January 2017,” commented Steve Cartt, President & Chief Executive Officer.
About the SCiStar Trial
The SCiStar trial is testing three sequential escalating doses of AST-OPC1 administered at up to 20 million AST-OPC1 cells in as many as 35 patients with sub-acute, C-5 to C-7, motor complete (AIS-A or AIS-B) cervical SCI. These individuals have essentially lost all movement below their injury site and experience severe paralysis of the upper and lower limbs. AIS-A patients have lost all motor and sensory function below their injury site, while AIS-B patients have lost all motor function but may retain some minimal sensory function below their injury site. AST-OPC1 is being administered 14 to 30 days post-injury. Patients will be followed by neurological exams and imaging procedures to assess the safety and activity of the product. Additional information on the Phase 1/2a trial, including trial sites, can be found at www.clinicaltrials.gov, using Identifier NCT02302157, and at the SCiStar Study Website (www.scistar-study.com).
Asterias previously announced that it had been granted FDA clearance to expand patient enrollment in the Phase 1/2a clinical trial from 13 patients to up to 35 patients, based on the continued favorable safety profile observed in the ongoing clinical study. The Company believes that this change will increase the statistical confidence of the safety and efficacy readouts, reduce the risks of the AST-OPC1 program and position the product for potential accelerated regulatory approvals. Asterias has received a Strategic Partnerships Award grant from the California Institute for Regenerative Medicine, which provides $14.3 million of non-dilutive funding for the Phase 1/2a clinical trial and other product development activities for AST-OPC1.
More than 17,000 people sustain a spinal cord injury each year, but there are no FDA-approved therapeutics or devices that could potentially restore some function in individuals who have recently sustained a spinal cord injury.
About AST-OPC1
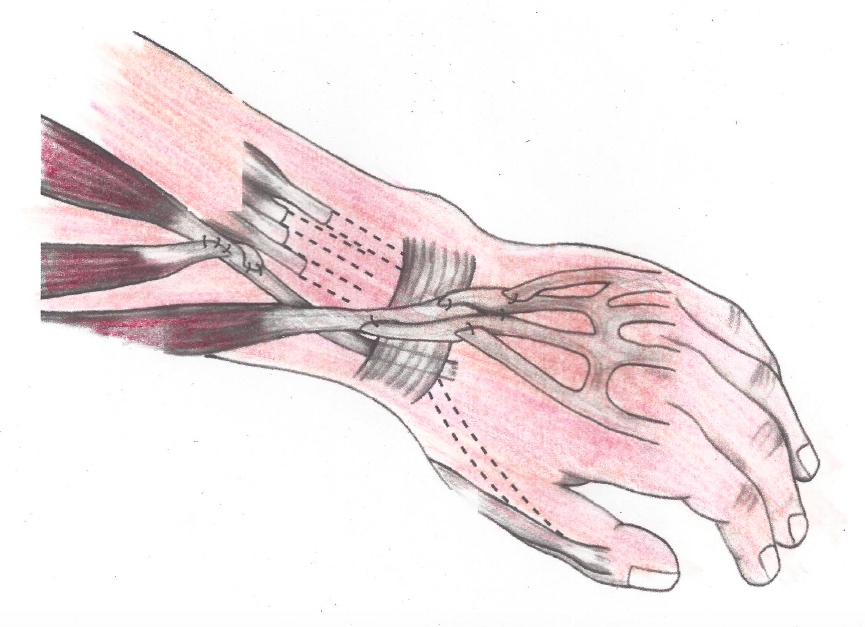
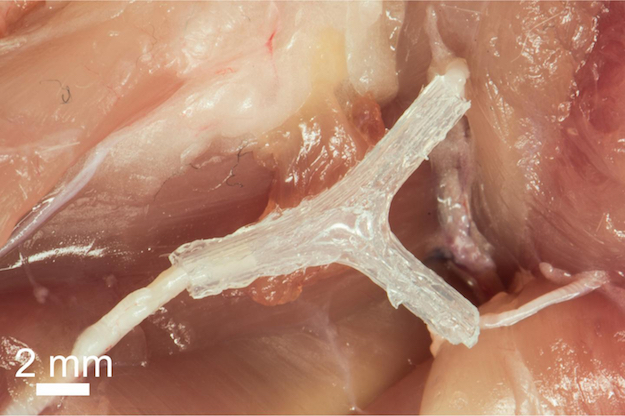
AST-OPC1, an oligodendrocyte progenitor population derived from human embryonic stem cells, has been shown in animals and in vitro to have three potentially reparative functions that address the complex pathologies observed at the injury site of a spinal cord injury. These activities of AST-OPC1 include production of neurotrophic factors, stimulation of vascularization, and induction of remyelination of denuded axons, all of which are critical for survival, regrowth and conduction of nerve impulses through axons at the injury site. In preclinical animal testing, AST-OPC1 administration led to remyelination of axons, improved hindlimb and forelimb locomotor function, dramatic reductions in injury-related cavitation and significant preservation of myelinated axons traversing the injury site.
In a previous Phase 1 clinical trial, five patients with neurologically complete, thoracic spinal cord injury were administered two million AST-OPC1 cells at the spinal cord injury site 7-14 days post-injury. They also received low levels of immunosuppression for the next 60 days. Delivery of AST-OPC1 was successful in all five subjects with no serious adverse events associated with the administration of the cells, with AST-OPC1 itself, or the immunosuppressive regimen. No evidence of rejection of AST-OPC1 was observed in detailed immune response monitoring of all patients. In four of the five patients, serial MRI scans indicated that reduced spinal cord cavitation may have occurred. Based on the results of this study, Asterias received approval from FDA to progress testing of AST-OPC1 to patients with complete cervical spine injuries, which represents the first targeted population for registration trials.
About Asterias Biotherapeutics
Asterias Biotherapeutics, Inc. is a leading biotechnology company in the emerging field of regenerative medicine. The company’s proprietary cell therapy programs are based on its immunotherapy and pluripotent stem cell platform technologies. Asterias is presently focused on advancing three clinical-stage programs which have the potential to address areas of very high unmet medical need in the fields of oncology and neurology. AST-OPC1 (oligodendrocyte progenitor cells) is currently in a Phase 1/2a dose escalation clinical trial in spinal cord injury. AST-VAC1 (antigen-presenting autologous dendritic cells) is being evaluated by Asterias for further development after demonstrating promise in a Phase 2 study in Acute Myeloid Leukemia (AML) and completing a successful end-of-Phase 2 meeting with the FDA. AST-VAC2 (antigen-presenting allogeneic dendritic cells) represents a second generation, allogeneic immunotherapy. The company’s research partner, Cancer Research UK, plans to begin a Phase 1/2 clinical trial of AST-VAC2 in non-small cell lung cancer in 2017. Additional information about Asterias can be found at www.asteriasbiotherapeutics.com.
FORWARD-LOOKING STATEMENTS
Statements pertaining to future financial and/or operating and/or clinical research results, future growth in research, technology, clinical development, and potential opportunities for Asterias, along with other statements about the future expectations, beliefs, goals, plans, or prospects expressed by management constitute forward-looking statements. Any statements that are not historical fact (including, but not limited to statements that contain words such as “will,” “believes,” “plans,” “anticipates,” “expects,” “estimates”) should also be considered to be forward-looking statements. Forward-looking statements involve risks and uncertainties, including, without limitation, risks inherent in the development and/or commercialization of potential products, uncertainty in the results of clinical trials or regulatory approvals, need and ability to obtain future capital, and maintenance of intellectual property rights. Actual results may differ materially from the results anticipated in these forward-looking statements and as such should be evaluated together with the many uncertainties that affect the businesses of Asterias, particularly those mentioned in the cautionary statements found in Asterias’ filings with the Securities and Exchange Commission. Asterias disclaims any intent or obligation to update these forward-looking statements.
SOURCE Asterias Biotherapeutics, Inc.
Related Links
http://www.asteriasbiotherapeutics.com