SAN DIEGO, March 16, 2017 /PRNewswire-USNewswire/ — The Kappa Delta Sorority and the Orthopaedic Research and Education Foundation (OREF) today presented four awards to scientists conducting outstanding musculoskeletal disease or injury research with the goal of advancing patient treatment and care. Honored at the 2017 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS), these award winners have made invaluable discoveries in:
- Using lower extremity biomechanics in patients with ankle osteoarthritis and ankle arthroplasty to direct clinical care;
- Advancing precision medicine for clubfoot treatment through basic research;
- Kinematics of the normal and injured wrist: the importance of the midcarpal joint; and
- The impact of arthroplasty implant registries over the past five decades.
Using lower extremity biomechanics in patients with ankle osteoarthritis and ankle arthroplasty to direct clinical care
The 2017 Kappa Delta Young Investigator Award was presented to Robin Queen, PhD, FACSM, associate professor of biomedical engineering and mechanics at Virginia Tech in Blacksburg, Va., and associate professor of orthopaedic surgery at Virginia Tech Carilion School of Medicine for her research on the impact of ankle osteoarthritis and total ankle replacement on gait mechanics and balance.
Each year, there are approximately 50,000 new cases of ankle osteoarthritis, a debilitating disease that leads to profound skeletal and functional changes, including deformity, severe and recurrent pain, cartilage breakdown and gait dysfunction. Because of the new generation of implants, this was a critical time to examine the impact of ankle osteoarthritis and total ankle arthroplasty on total body mechanics and function. Dr. Queen examined the impact of ankle osteoarthritis and ankle replacement on balance, ankle range of motion, patient outcomes, and movement symmetry to improve long-term health and function.
“It was important for us to understand this patient population in a way that we never have, and to improve their quality of life post surgery, while decreasing the need for additional surgeries,” said Dr. Queen. “We are working to change the way surgeons look at patient recovery. We want them to examine movement and physical performance, not just patient reported outcomes. We need to begin to address the impact that ankle disease and surgery has on the entire body through a more holistic approach as we advance postoperative care in order to improve long-term health and mobility.”
Dr. Queen hopes this research will emphasize the importance of assessing measures like physical performance and not just patient recorded outcomes to assess recovery and to determine what additional postoperative intervention programs are necessary for individual patients.
Advancing personalized medicine for clubfoot through translational research
The 2017 Kappa Delta Ann Doner Vaughn Award was presented to Matthew Dobbs, MD, for his research on advancing personalized medicine for clubfoot. Dr. Dobbs is the Dr. Asa C. and Mrs. Dorothy W. Jones professor of orthopaedic surgery at Washington University in St. Louis. The research was co-authored by Christina Gurnett, MD, PhD, professor Department of Neurology and Division of Pediatric Neurology at Washington University School of Medicine.
Clubfoot is one of the most common pediatric orthopaedic disorders with an estimated one per 1,000 live births. If left untreated, it can result in foot and leg deformities, pain that limits mobility and social stigma. While the Ponseti method has revolutionized clubfoot treatment, it’s not effective for all patients.
Twenty-five percent of patients with clubfoot have a family history of clubfoot. Dr. Dobbs and his wife, Dr. Gurnett co-founded the Musculoskeletal Genetics Laboratory at Washington University where they leveraged scientific advances including human gene sequencing, molecular genetic engineering of mouse models and magnetic resonance imaging (MRI), as well as new treatment technologies to understand and target specific abnormalities.
Their work helped discover mutations in the PITX1, TBX4 and HOXC genes that cause familial clubfoot and vertical talus. And since no one had used MRI to examine the legs of clubfoot patients, they began to look for hypomorphic muscle, bone and vasculature differences in patients.
“Not all cases of clubfoot are the same, so it doesn’t make sense to treat everyone the same,” said Dr. Dobbs. “To improve the lives of all children with clubfoot, we believe it’s critical not only to understand the genetic and morphological abnormalities contributing to foot development, but also to use this information to devise personalized treatment paradigms.”
They started a large, multi-center, randomized clinical trial, to help predict response to treatment and find ways to alter treatment to make it even more effective. Their research has led to the creation of an algorithm to develop to a new classification system; improved brace design to improve patient compliance with the development of the Dobbs foot abduction brace; optimized treatment methods for neglected and syndromic clubfoot; and a new non-operative treatment for congenital vertical talus called the Dobbs method.
“Receiving this award is a true honor. It is our hope that we can continue to develop personalized therapies that minimize the extent of surgery by addressing specific muscular, skeletal, vascular or neuronal abnormalities,” said Dr. Dobbs.
Kinematics of the normal and injured wrist: the importance of the midcarpal joint
Scott W. Wolfe MD, chief emeritus of hand surgery and attending orthopaedic surgeon at the Hospital for Special Surgery in New York City, received the 2017 Kappa Delta Elizabeth Winston Lanier Award for his research titled “Kinematics of the normal and injured wrist: the importance of the midcarpal joint.” The research was co-authored by Joseph J. (Trey) Crisco, III, PhD, Henry F. Lippitt professor of orthopaedics and professor of Engineering (Research) at Brown University.
The eight carpal bones that comprise the wrist joint represent the most complex articular system in the human body–each capable of moving in different degrees or directions dependent on the position, motion and force generation of the hand in space. Any instability of the wrist caused by injury can generate disabling symptoms that prevent normal daily or occupational activities and lead to debilitating, degenerative arthritis in a very short time.
“Our work can be described in three stages, roughly corresponding to the three decades of our collaborative efforts, namely, 1990s: development of non-invasive technology to measure normal carpal bone kinematics during wrist motion; 2000s: application of that technology to understand “functional” kinematics of the normal and injured wrist; and 2010s: conceptualization and development of improved methods for treatment of degenerative arthritis based on our understanding of functional kinematics,” said Dr. Wolfe.
Dr. Wolfe has long recognized the dramatic evolution of computed tomography (CT) and its application to 3D visualization of small bones and joint fractures about the upper limb. Within five years of starting their research, they were able to generate movies of individual wrist bones moving–something that had never been done before–by using the latest CT equipment and advanced technology developed by Dr. Crisco.
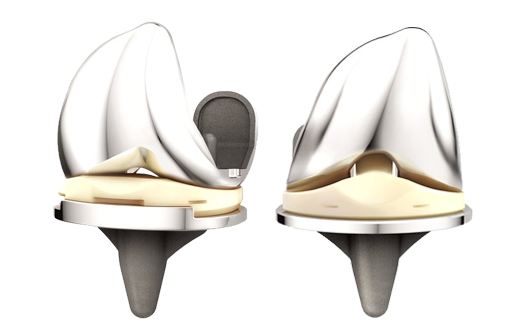
In addition to being the first to map the wrist’s movement in the dart thrower’s motion, they were then able to create devices to treat wrist instability including the novel midcarpal total wrist arthroplasty system, which is currently pending FDA approval. Their midcarpal kinematic hemi-arthroplasty has already received CE approval and is currently used in the U.K.
“This award means an enormous amount to us,” said Dr. Wolfe. “It validates what we’ve done for three decades, cements the importance of our research to orthopaedic and clinical care of patients, and it energizes us to double down and take this to the next step.”
Drs. Wolfe and Crisco have already applied for grants to continue their research initiatives.
Arthroplasty implant registries over the past five decades: development, current and future impact
The 2017 OREF Clinical Research Award was presented to Henrik Malchau, MD, PhD-professor of orthopaedics at Harvard Medical School and vice chief orthopaedics and co-director of the Harris Orthopaedic Laboratory Massachusetts General Hospital in Boston-for his research studying the impact of arthroplasty implant registries throughout the world. The research was co-authored by Daniel Berry, MD; Charles Bragdon, PhD; Göran Garellick, MD, PhD; William H. Harris, MD, ScD; Peter Herberts, MD, PhD; Johan Kärrholm, MD, PhD; David Lewallen, MD; Lars Lidgren, MD, PhD; and Otto Robertson, MD, PhD.
The development of arthroplasty registries in Sweden and the United States has promoted the concept of evidence-based medicine over the past 50 years. The Mayo Clinic Total Joint Registry and the Harris Joint Registry (Massachusetts General Hospital) have greatly contributed to the advancement of arthroplasty surgery, and have served as an important role of identifying poorly performing implants and techniques in the U.S.
The Swedish Knee Arthroplasty Registry and the Swedish Hip Arthroplasty Registry have established the infrastructure, analysis and reporting mechanisms and leadership that have enabled other countries to develop registries around the world.
“I have spent my entire career developing and promoting the use of registries to collect regional, national and global data,” said Dr. Malchau. “As a result, we have been able to identify medical devices and practices that have high rates of failure, while promoting best practices for arthroplasty patients. These registries have supplied the scientific bases for decision making in literally all aspects of arthroplasty patient care.”
As a result of this research, there are now international efforts underway to promote and increase collaboration among various national registries, including the American Joint Replacement Registry to pool data, establish standards and guidelines, and to develop a system of early detection and warning regarding practices and implants that exhibit inferior performance.
About the Kappa Delta Awards
In 1947, at its golden anniversary, the Kappa Delta Sorority established the Kappa Delta Research Fellowship in Orthopaedics, the first award ever created to honor achievements in the field of orthopaedic research. The first annual award, a single stipend of $1,000, was made available to the Academy in 1949 and presented at the AAOS meeting in 1950. The Kappa Delta Awards have been presented by the Academy to persons who have performed research in orthopaedic surgery that is of high significance and impact.
The sorority has since added two more awards and increased the award amounts to $20,000 each. Two awards are named for the sorority national past presidents who were instrumental in the creation of the awards: Elizabeth Winston Lanier and Ann Doner Vaughn. The third is known as the Young Investigator Award.
The fourth award, also providing $20,000, is the OREF Clinical Research Award. Established in 1995, the award recognizes outstanding clinical research related directly to musculoskeletal disease or injury. All submitted manuscripts are reviewed, graded, and selected by the American Academy of Orthopaedic Surgeons’ Research Development Committee. For more information about the manuscript submission process, please visit aaos.org/kappadelta.
Previous Kappa Delta and OREF Clinical Research Award winners
The American Academy of Orthopaedic Surgeons
With more than 39,000 members, the American Academy of Orthopaedic Surgeons (AAOS) is the world’s largest medical association of musculoskeletal specialists. The AAOS provides education programs for orthopaedic surgeons and allied health professionals, champions and advances the highest quality musculoskeletal care for patients, and is the authoritative source of information on bone and joint conditions, treatments and related issues.
Visit AAOS at:
Newsroom.aaos.org for bone and joint health news, stats, facts, images and interview requests.
ANationinMotion.org for inspirational patient stories, and orthopaedic surgeon tips on maintaining bone and joint health, avoiding injuries, treating musculoskeletal conditions and navigating recovery.
Orthoinfo.org for patient information on hundreds of orthopaedic diseases and conditions.
Facebook.com/AAOS1
CONTACT: Kayee Ip, 312-543-3211, 847-384-4035, ip@aaos.org; Lauren P. Riley, 708-227-1773, 847-384-4031, pearson@aaos.org
This information is being sent to you by:
American Academy of Orthopaedic Surgeons
9400 W. Higgins Road, Rosemont, IL , 60018,
http://www.aaos.org