BELGRADE, Mont., Sept. 12, 2017 (GLOBE NEWSWIRE) — Xtant Medical Holdings, Inc. (NYSE American:XTNT), a leader in the development of regenerative medicine products and medical devices, today announced that the U.S. Food and Drug Administration (FDA) has cleared product line extensions for the Irix-A interbody spacer. The clearance provides for the addition of three additional size configurations for an expanded market opportunity, and importantly, for use with allograft. This clearance is the second received during this quarter, and continues to strengthen Xtant Medical’s focus in providing a more comprehensive portfolio focused on regenerative care for the patient.
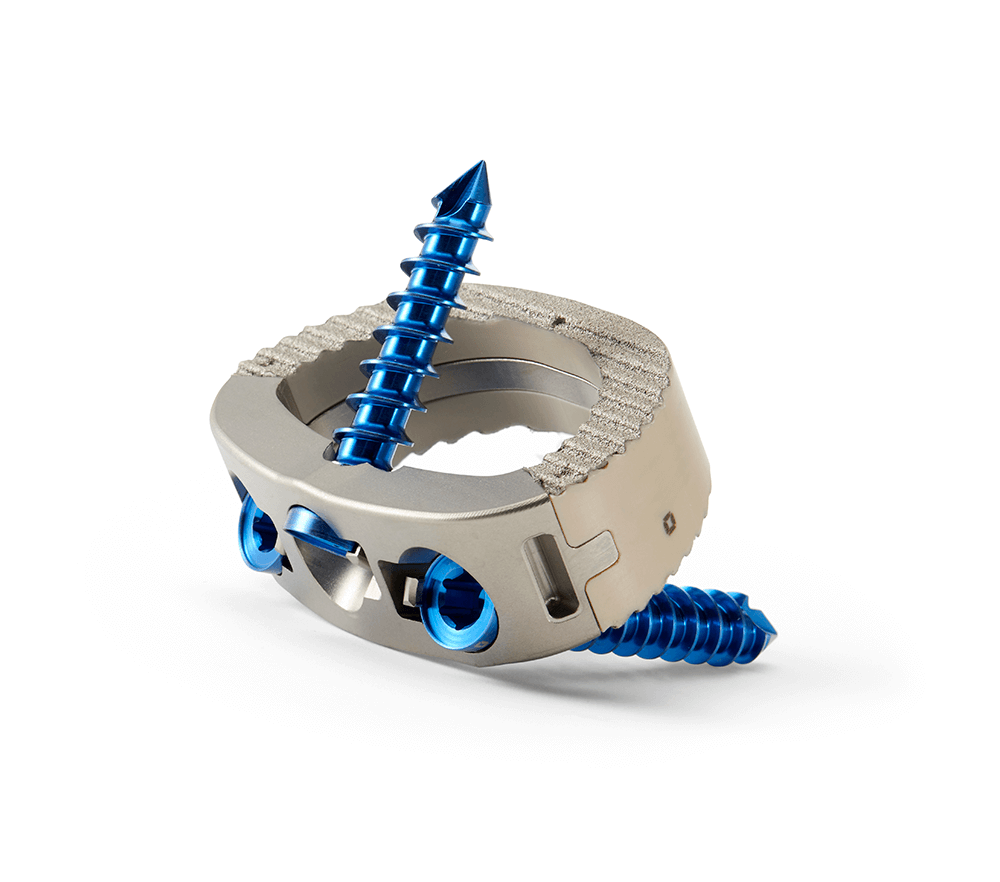
Xtant Medical’s Irix-A is a standalone interbody device used in anterior lumber interbody fusions. The current product line offers a titanium and PEEK composite implant, with the additional option of a titanium plasma coating for improved osseointegration with the spinal endplate, all with 8° or 12° of lordosis for alignment with the curvature of the spine. This new 510k clearance adds three additional degrees of lordosis, specifically 16°, 20°, and 24°, providing the surgeon with a wider variety of choices to correct the patient’s loss of lordosis and to improve sagittal balance. The FDA clearance also expands the indications of use to include use with allograft, such as Xtant Medical’s patented OsteoSponge, proprietary 3Demin, or OsteoVive viable cell allograft.
“The clearance of the additional footprints, including hyperlordotic options, further enhances our lumbar product portfolio in response to our customer’s needs,” said Gregory Juda, Chief Scientific Officer. “We continue to execute on our focus of combining our hardware and biologics technologies, strengthening our position as a comprehensive supplier for spine surgeons and their patients.”
The Irix-A Lumbar Integrated Fusion System consists of an integrated titanium ring, surrounded by an outer PEEK ring and three screws. It is intended for anterior spinal fusion procedures at one or two contiguous levels of the lumbosacral spine (L2-S1 inclusive) in skeletally mature patients for the treatment of degenerative disc disease.
Xtant Medical estimates the US market for standalone anterior lumbar interbody fusion market to be approximately $230 million and growing. The US market for Demineralized Bone Matrix (DBM) is estimated at $410M. The additional Irix-A interbody implants are intended to be available to customers later this year.
About Xtant Medical
Xtant Medical Holdings, Inc. (NYSE American:XTNT) develops, manufactures and markets class-leading regenerative medicine products and medical devices for domestic and international markets. Xtant products serve the specialized needs of orthopedic and neurological surgeons, including orthobiologics for the promotion of bone healing, implants and instrumentation for the treatment of spinal disease, tissue grafts for the treatment of orthopedic disorders, and biologics to promote healing following cranial, and foot and ankle surgeries. With core competencies in both biologic and non-biologic surgical technologies, Xtant can leverage its resources to successfully compete in global neurological and orthopedic surgery markets. For further information, please visit www.xtantmedical.com.
Important Cautions Regarding Forward-looking Statements
This press release contains certain disclosures that may be deemed forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995 that are subject to significant risks and uncertainties. Forward-looking statements include statements that are predictive in nature, that depend upon or refer to future events or conditions, or that include words such as “continue,” “efforts,” “expects,” “anticipates,” “intends,” “plans,” “believes,” “estimates,” “projects,” “forecasts,” “strategy,” “will,” “goal,” “target,” “prospects,” “potential,” “optimistic,” “confident,” “likely,” “probable” or similar expressions or the negative thereof. Statements of historical fact also may be deemed to be forward-looking statements. We caution that these statements by their nature involve risks and uncertainties, and actual results may differ materially depending on a variety of important factors, including, among others: the ability to comply with covenants in the Company’s senior credit facility and to make deferred interest payments; the ability to maintain sufficient liquidity to fund operations; the ability to remain listed on the NYSE MKT; the ability to obtain financing on reasonable terms; the ability to increase revenue; the ability to continue as a going concern; the ability to maintain sufficient liquidity to fund operations; the ability to achieve expected results; the ability to remain competitive; government regulations; the ability to innovate and develop new products; the ability to obtain donor cadavers for products; the ability to engage and retain qualified technical personnel and members of the Company’s management team; the availability of Company facilities; government and third-party coverage and reimbursement for Company products; the ability to obtain regulatory approvals; the ability to successfully integrate recent and future business combinations or acquisitions; the ability to use net operating loss carry-forwards to offset future taxable income; the ability to deduct all or a portion of the interest payments on the notes for U.S. federal income tax purposes; the ability to service Company debt; product liability claims and other litigation to which we may be subjected; product recalls and defects; timing and results of clinical studies; the ability to obtain and protect Company intellectual property and proprietary rights; infringement and ownership of intellectual property; the ability to remain accredited with the American Association of Tissue Banks; influence by Company management; the ability to pay dividends; and the ability to issue preferred stock; and other factors.
Additional risk factors are listed in the Company’s Annual Report on Form 10-K and Quarterly Reports on Form 10-Q under the heading “Risk Factors.” The Company undertakes no obligation to release publicly any revisions to any forward-looking statements to reflect events or circumstances after the date hereof or to reflect the occurrence of unanticipated events, except as required by law.
Investor Contact
CG CAPITAL
Rich Cockrell
877.889.1972
investorrelations@cg.capital
Company Contact
Xtant Medical
Molly Mason
mmason@xtantmedical.com