Oct 18, 2016 – NOBLESVILLE, Ind. –(BUSINESS WIRE)
Nexxt Spine, LLC, a privately held medical device company dedicated to increasing procedural efficiency and clinical outcomes for patients with debilitating spinal conditions, further demonstrates the company’s on-going commitment toward reducing post-operative surgical infections with the addition of an ISO Class 10,000 (International Standards Organization) Certified Cleanroom for pre-packaging sterile spinal implants within their manufacturing and corporate headquarters located in Noblesville, IN.
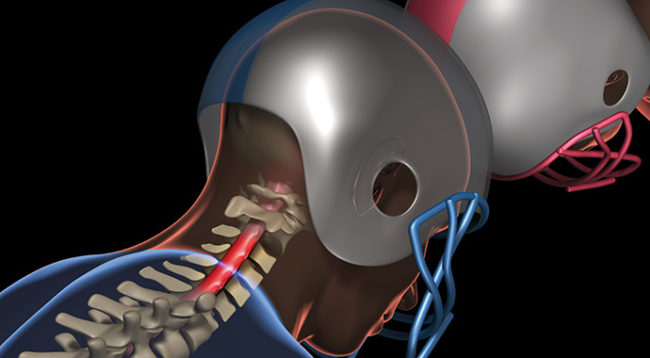
Postoperative spine infections have been reported to occur in 1 to 15% of patients after spine surgery. A study of 105 consecutive spine surgeries published in The Spine Journaldemonstrated that spinal implants sterilized following a validated hospital protocol were tested and found to have a contamination rate of 16.7%1.
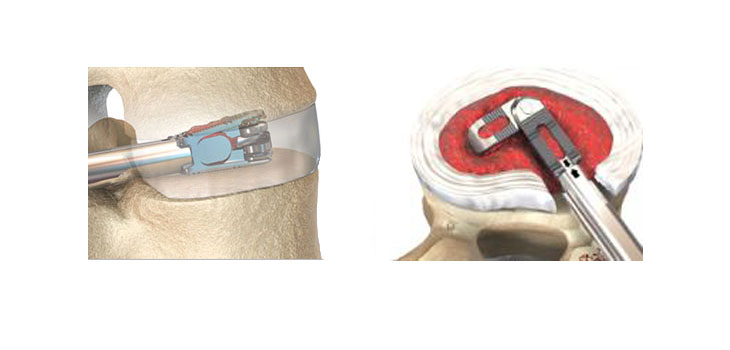
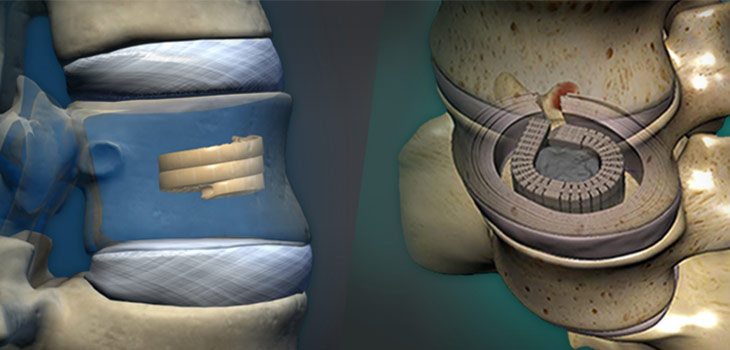
“Patient safety is our #1 priority. While multiple factors could contribute to post-operative infection, the authors published data on spinal implants previously assumed sterile and later found to be contaminated,” reports Dr. Robert Wertz, V.P. New Product Development at Nexxt Spine. “We have recently completed certification and validation of our ISO 7, Class 10,000 Cleanroom and will launch our pre-packaged sterile implant initiative parallel to the anticipated FDA clearance of Nexxt Matrixx, a 3-D printed, porous, titanium line of intervertebral spacers used in spine fusion procedures.”
According to Nexxt Spine’s President, Andy Elsbury, “Pre-packaged sterile implants do not require disinfection and steam sterilization prior to use. Implants are individually wrapped in a peel pack tray and sterilized using electron beam (E-beam) radiation. Implant packaging is opened literally seconds prior to implantation. Unlike the reprocessed spinal implants referenced in The Spine Journal study, the risk for implant contamination is virtually non-existent.”
Nexxt Spine will be exhibiting at the 31st Annual North American Spine Society (NASS) Meeting, October 26-29, 2016, in Boston, MA. To arrange an introductory meeting with a member of Nexxt Spine’s Management Team please contact info@nexxtspine.com.
About Nexxt Spine
Nexxt Spine, LLC is a privately held medical device manufacturer dedicated to increasing procedural efficiency and patient outcomes through development of innovative products, manufactured on the most technologically advanced platforms, and utilizing irreproachable quality standards to treat painful and debilitating spinal pathologies.
Additional information is available online at www.nexxtspine.com.
Reference:
1. Bible, J. E., O’Neill, K. R., Crosby, C. G., Schoenecker, J. G., McGirt, M. J., & Devin, C. J. (2013). Implant contamination during spine surgery. The Spine Journal, 13(6), 637–640. doi:10.1016/j.spinee.2012.11.053
View source version on businesswire.com:http://www.businesswire.com/news/home/20161018005323/en/
Nexxt Spine, LLC
Sarah Caito Koch, 317-436-7801
Scaito@NexxtSpine.com
Copyright Business Wire 2016
This article was originally distributed via Business Wire. Business Wire, Frankly and this Site make no warranties or representations in connection therewith. If you are affiliated with this page and would like it removed please contact pressreleases@franklyinc.com