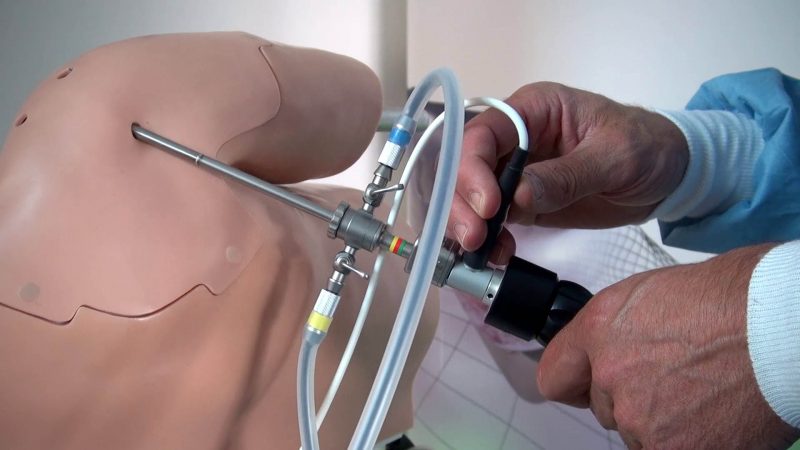
NEW YORK, Jan. 29, 2018 /PRNewswire/ — Paradigm Spine, LLC, a leader in providing motion preservation solutions for the treatment of lumbar spinal stenosis, today announced publication of the ESCADA 2-year trial results (European Study of coflex And Decompression Alone) in the January 2018 issue of the Journal of Neurosurgery Spine (JNS), official journal of the American Association of Neurological Surgeons (AANS). ESCADA reports a prospective, randomized, controlled, multi-center trial comparing decompression alone to decompression with coflex® Interlaminar Stabilization® for treatment of moderate to severe lumbar spinal stenosis. coflex is the first and only motion preserving minimally invasive treatment for moderate to severe spinal stenosis post decompression. A total of 225 patients were enrolled in the study with 91% follow up at 2 years.
The study authors concluded that decompression with coflex Interlaminar Stabilization extends the durability and sustainability of a decompression procedure.
“These data strongly validate for the surgical spine community that coflex is a safe and effective protector of a decompression procedure,” said Marc Viscogliosi, President and CEO of Paradigm Spine. “This means that surgeons treating patients with lumbar spinal stenosis can be more confident than ever in their treatment options, knowing that a randomized controlled trial has demonstrated with statistical significance that nearly twice as many patients with decompression alone have a risk of secondary intervention as compared to coflex patients. coflex is the first and only lumbar spinal device that has produced the highest level of evidence in two separate prospective, randomized, controlled studies against two different control groups – which exhibits the thoroughness and reproducibility of these findings. There is now potentially a more effective surgical option between the two typical treatments for lumbar spinal stenosis, and we are proud to lead the way in changing the standard of care for surgeons and their patients with this diagnosis.”
Highlights of ESCADA results:
- The rate of patients achieving Composite Clinical Success was statistically superior in the coflex group vs. the Decompression Alone group (p=0.017)
- Patients who received Decompression Alone experienced significantly more loss of foraminal and posterior disc height maintenance compared to the coflex group (p<0.001)
- The Decompression Alone group experienced 228% more subsequent epidural steroid injections compared to the coflex group (p=0.0065)
- coflex patients experienced 2.4 times more improvement in walking distance measurements compared to Decompression Alone patients (p=0.062)
- At 24 months, the Decompression Alone group was 1.4 times more likely to be taking opioids compared to the coflex group
The ESCADA trial included seven sites in Europe / Germany with a total of 225 patients who were randomized to either decompression alone (DA, control group) or decompression with coflex Interlaminar Stabilization (coflex, study group). Overall trial success was based on a combined outcome measure called Composite Clinical Success (CCS), in which all four components must be met: 1) ODI success with improvement > 15 points; 2) survivorship with no secondary surgical interventions or lumbar injections; 3) neurologic maintenance or improvement without worsening; 4) no device-related severe adverse events. This is the same success criteria that was used in the U.S. IDE study of coflex that has published 5-year follow-up, allowing some direct comparisons to be drawn between the cohorts representing 547 patients collectively. Secondary measures were also collected such as walking distance, foraminal and disc height maintenance, leg and back pain scores, and opioid use.
“With the important work of the ESCADA trial, we can see that coflex extends the success and durability of a decompression procedure for lumbar spinal stenosis, while still allowing natural motion to occur,” says ESCADA author and Principal Investigator Professor Michael Rauschmann. “The U.S. IDE study first investigated and defined the long-term problems with lumbar fusion procedures that can be alleviated with coflex. And now, through this controlled trial, we can begin to answer the questions of the sustainability of decompression alone, and the need to provide additional stabilization for those patients with coflex at first surgical intervention to avoid future complications.”
Journal of Neurosurgery Spine. January 2018. Volume 28, Issue 1 (http://thejns.org/doi/full/10.3171/2017.11.SPINE17643).
About Lumbar Spinal Stenosis (LSS)
Lumbar spinal stenosis (LSS), affecting 1.6 million patients annually in the United States, is a debilitating and degenerative disease often associated with significant leg and back pain, leg numbness and weakness, and significant reduction in an active lifestyle. Historically, the two traditional surgical treatment options for LSS included decompression alone or decompression with lumbar fusion. Decompression alone has proven effective at relieving pain symptoms caused by lumbar spinal stenosis, however, patients may not experience long term symptomatic relief, resulting in subsequent epidural injections for pain management, or additional surgeries for conversion to a fusion. Decompression with fusion has proven to provide pain relief and stabilize the diseased segment, but may lead to adjacent level disease requiring subsequent surgeries.
About Paradigm Spine, LLC:
Paradigm Spine, LLC, founded in 2004, is a privately held company and remains focused on the design and development of solutions for the disease management of spinal stenosis. The Company’s signature product is the coflex® Interlaminar Stabilization® device, which is currently used in over 50 countries worldwide. coflex is the only lumbar spinal device that has produced Level I evidence in two separate prospective, randomized, controlled studies against two different control groups, changing the standard of care for lumbar spinal stenosis treatment. For additional information visit www.paradigmspine.com or www.coflexsolution.com.
SOURCE Paradigm Spine, LLC